Vulvovaginitis

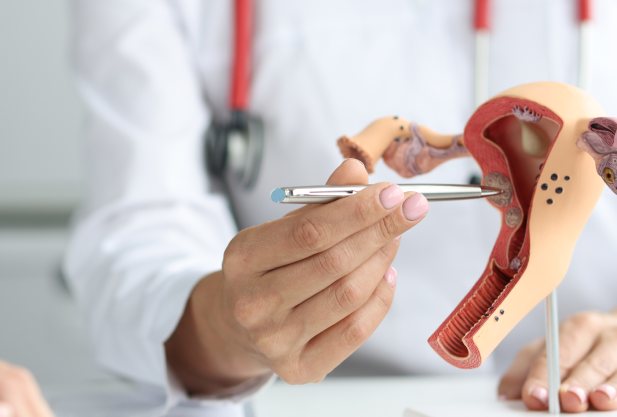
specialists

equipment

treatment
Symptoms of vulvovaginitis

Symptoms of vulvovaginitis:
- Itching and burning. Often begin as the first signs of inflammation. Itching can be so severe that it interferes with normal movement or rest. The burning is intensified by contact with urine or the use of inappropriate hygiene products
- Redness and swelling. The skin and mucous membranes become red, swollen and inflamed. These changes are the body's reaction to irritation or infection
- Unusual discharge. The discharge increases in volume, its color and odor change. For example, with bacterial vaginosis, the discharge may have a characteristic "fishy" odor, and with candidiasis it becomes thick and white, similar to cottage cheese
- Pain when urinating. Often women complain of pain or burning when visiting the toilet. This is due to inflammation of the mucous membrane and is sometimes accompanied by a urinary tract infection
- Discomfort during sexual intercourse. The mucous membrane becomes more sensitive, which can cause painful sensations or even sharp pain during intimacy
- Dryness and a feeling of tightness. More common in women during menopause due to a decrease in estrogen levels. The mucous membrane loses its elasticity and becomes easily injured and irritated
In case of severe inflammation, weakness, fever and enlarged lymph nodes in the groin may appear.
Treatment of vulvovaginitis
Drug treatment
The first step in treating vulvovaginitis is to eliminate the cause of the inflammation. If the disease is caused by bacteria, the doctor prescribes antibiotics. For example, for bacterial vaginosis, metronidazole is used, which affects gardnerella and other pathogens. Medicines can be in the form of suppositories, creams or tablets, depending on the severity of the symptoms. For fungal infections, such as candidiasis, antifungal drugs are used, for example, fluconazole or clotrimazole. These drugs help relieve itching, burning and reduce the amount of discharge. In the case of viral infections, such as herpes, acyclovir is included in the therapy, which suppresses the activity of the virus and accelerates healing.
Conservative methods
When vulvovaginitis is caused not by an infection, but by an allergic reaction or age-related changes, the treatment is different. For example, menopausal women often develop atrophic vulvovaginitis due to a decrease in estrogen levels. In such cases, hormonal creams and suppositories are used to moisturize the mucous membrane, reduce dryness and eliminate discomfort. If the cause is associated with external irritants, such as synthetic underwear or aggressive hygiene products, it is enough to eliminate these factors to alleviate the condition. Doctors may also recommend probiotics to restore the vaginal microflora, especially after a course of antibiotics.
Additional methods
Additional measures may be used to speed up recovery and prevent complications. For example, physiotherapy — laser or ultrasound — improves blood circulation in the pelvic area, which promotes tissue healing. In women suffering from chronic forms of vulvovaginitis, such methods often give good results. In addition, the doctor may recommend special exercises to strengthen the pelvic floor muscles, especially if the disease is associated with age-related changes or childbirth.
Complications of vulvovaginitis
Without treatment, vulvovaginitis can lead to serious problems. The infection easily spreads to neighboring organs, such as the bladder, causing cystitis. This is accompanied by burning, frequent urge to go to the toilet and pain.
Another danger is the transition of the disease to a chronic form. In this case, the symptoms become weaker, but the inflammation remains. Frequent exacerbations occur due to stress, decreased immunity or poor hygiene. Chronic vulvovaginitis worsens the quality of life and creates a risk of new infections, such as inflammation of the uterus or appendages.
It is important not to delay contacting a doctor. The sooner treatment is started, the less likely complications are.
-
Cystitis
Pain and burning when urinating, constant feeling of urge.
-
Chronic inflammation
A constant irritation that is difficult to cure.
-
Frequent relapses
The infection returns again and again, disrupting the microflora.
-
Inflammation of the appendages
Spread to the uterus and tubes can lead to infertility.
-
Scar formation
The affected tissues may change structure, which causes discomfort.
General information
Answers to popular questions
Doctors of the K+31 clinic (Moscow) provide answers to the most pressing questions of patients.
What to do if symptoms return?
Recurring symptoms often indicate that the cause of the disease has not been eliminated. You need to see a doctor to adjust the treatment and additional diagnostics, such as checking the microflora or testing for latent infections.
Is it possible to do without medication?
If the cause is irritation from chemicals or allergies, eliminating the provoking factor may help. But with infections, you can't do without medication. Self-medication will only make the problem worse.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services

















































What is vulvovaginitis?
Vulvovaginitis is an inflammatory disease affecting the external genitalia (vulva) and the mucous membrane of the vagina. It can occur in women of any age, but more often occurs in those who are in the reproductive period. The main reason is most often a violation of the vaginal microflora or the effect of external stimuli.