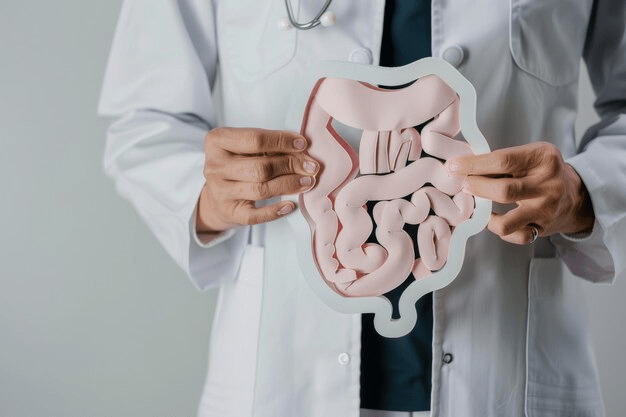
Clostridial Colitis

specialists

equipment

treatment
Additional risk factors

In addition to antibiotic treatment, there are other factors that can increase the risk of developing clostridial colitis. These include:
- Long-term hospital treatment
- Advanced age
- Recent abdominal surgery
- Weak immunity
- Malignant tumors
- Renal failure
Sometimes the disease develops in patients with chronic obstructive pulmonary diseases. Another provoking factor is the use of H2-histamine receptor blockers and proton pump inhibitors.
Pseudomembranous colitis: symptoms
Mild form of pseudomembranous colitis
- Diarrhea. The most common symptom, in which the stool can be profuse and watery, sometimes with mucus
- Abdominal pain. Patients are bothered by cramping pain
- Clostridiosis. Accompanied by fever, weakness, headache, nausea and vomiting
If the disease progresses, additional symptoms may appear, which continue even after stopping antibiotics.
Additional symptoms
- Antibiotic-associated yellow or green diarrhea
- Presence of mucus and blood in the stool
- Metabolic disorders due to dehydration and water-electrolyte imbalance
In addition, patients experience weakness, rapid pulse, low blood pressure, as well as impaired muscle tone and paresthesia.
Features of severe pseudomembranous enterocolitis
- Rapid development. Symptoms develop faster, intoxication increases, abdominal pain becomes more intense, and blood in the stool appears from the first days of the disease
- Complications. Pathological expansion of the intestine (megacolon) may occur, which leads to rupture of the intestine and the development of peritonitis
Antibiotic-associated colitis (clostridium ramosum) requires immediate treatment. If you notice the above symptoms in yourself or a loved one, consult a doctor immediately.
General information

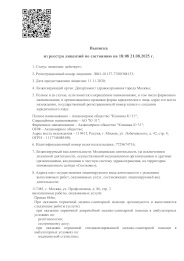
This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services


































Causes of the disease
Clostridium is a bacteria naturally present in the intestines of many humans and animals. Under normal conditions, it coexists with other bacteria without causing any health problems. When the microflora balance is disrupted, C. difficile becomes active, begins to actively multiply, and secrete toxins. These toxins damage the intestinal mucosa and cause inflammation, leading to the development of clostridial colitis.
The Effect of Antibiotics on Intestinal Microflora
Antibiotics are widely used in medicine to combat bacterial infections. While they kill harmful microorganisms, they also affect beneficial bacteria, leading to intestinal dysbiosis. This creates favorable conditions for the active proliferation of C. difficile and the possible development of pseudomembranous colitis (ICD-10 code: A04.7).