Pancreatic cancer
Pancreatic cancer is a malignant tumor formed from the altered cells of the organ that secretes substances necessary for the digestion process and regulation of metabolism.

specialists

equipment

treatment
Types of pancreatic cancer

Based on its secretory function, the pancreas is divided into exocrine and endocrine parts. The exocrine part secretes digestive enzymes, which are released through ducts into the duodenum. Endocrine tissue secretes hormones that go directly into the blood. Depending on which of these tissues the tumor formed in, exocrine malignant tumors of the pancreas are distinguished (the most common) and endocrine.
The most common endocrine tumor is adenocarcinoma. It can be ductal (formed in the glandular cells of the pancreatic ducts - the most common form of cancer) or acinar-cell (from the cells of the acinus - a special structure of the pancreas).
In addition to adenocarcinoma, pancreatic cancer varieties include such rare types as squamous cell carcinoma, undifferentiated cancer, cystadenocarcinoma, adenosquamous carcinoma, signet ring cell carcinoma.
Benign tumors can form in the pancreas, such as intraductal papillary tumor or cystic mucinous tumor. But they can degenerate into malignant tumors, so they are often removed surgically, especially if their location interferes with the function of the pancreas. Patients with such diagnoses should be examined regularly.
Endocrine cell tumors occur in less than 5% of cases. They are called neuroendocrine tumors, as well as islet cell tumors. According to the hormone secreted by the cells responsible for the formation of the tumor, neoplasms are called: gastrinoma (a tumor of cells producing gastrin), insulinoma (insulin), glucagonoma (glucagon), somatostatinoma (somatostatin). Usually these are benign tumors of the pancreas, but there are also malignant ones.
In rare cases, malignant tumors in the pancreas are metastases from cancer in another organ - this is metastatic cancer. The primary tumor can be in the gastrointestinal tract, kidneys, lungs, mammary gland or prostate gland. Sometimes the pancreas can be affected by metastases of melanoma (skin and mucous membrane cancer), osteosarcoma (bone cancer), leiomyosarcoma (smooth muscle cancer), Merkel cell carcinoma (skin cancer).
Location of pancreatic cancer
Cancer of the head of the pancreas
This is the most common type of pancreatic cancer by localization. Tumors in this part are smaller than in the body and tail, but due to the bile duct that passes here, even a small tumor can become a serious problem. It can compress the duct, which causes mechanical jaundice. A neoplasm in the head of the pancreas can also lead to a narrowing of the lumen (stenosis) of the duodenum. Another complication of malignant tumors of this localization is bleeding due to tumor decay.
Pancreatic body cancer
In terms of prevalence of pancreatic tumors, its body is in second place. Neoplasms here are larger than in the head. They can lead to inflammation of the vessels (thrombophlebitis), blockage of the lumen of the vessels (phlebothrombosis) and even diabetes. Advanced forms of pancreatic cancer localized in the body of this organ can cause jaundice.
Pancreatic tail cancer
This is the rarest type of pancreatic cancer in terms of location. But it is more difficult to diagnose using ultrasound.

According to the international TNM system, pancreatic cancer is divided into stages depending on the characteristics of three indicators:
- T – the degree of growth of the primary tumor: T1 – a tumor that has affected only the tissues of the pancreas up to its capsule, T2 and T3 – tumors at different stages of growth into the capsule and surrounding tissues and organs.
- N – the number of affected lymph nodes: N0 – the lymph nodes are not affected by the tumor process, N1, N2 and N3 – cancer has affected a different (increasing) number of lymph nodes.
- M – the presence of distant metastases: M0 – there are none, M1 – there are.
According to these indicators and their values, four stages of pancreatic cancer can be distinguished:
- Stage 1 – T1N0M0;
- Stage 2 – T1N1M0;
- Stage 3 – T1N2M0, T2N0M0, T2N1M0;
- Stage 4 – any values of T or N, but necessarily M1.

All cancers are caused by mutations in cells. There are many risk factors that can trigger such mutations. The most common risk factors for pancreatic cancer are:
- Type 2 diabetes
- Chronic pancreatitis – various inflammatory processes in the pancreas
- Gallstone disease
- Liver cirrhosis
- Cysts or adenomas in the prostate gland
- Smoking and alcohol consumption
- Predominance of fatty and spicy foods in the diet
- Burdened heredity
- Excess weight, especially excess fat in the waist area
- Age – the risk increases after 45 years, and most often the disease occurs at the age of 70 years
Symptoms of pancreatic cancer
It should be noted that at the initial stages, the signs of the disease are almost imperceptible, most often the tumor begins to give symptoms only when it has grown and begun to spread in the body. The following symptoms may indicate the presence of the disease:
- Abdominal pain (upper part) that radiates to the back
- Pain during meals, in a horizontal position
- Loss of appetite
- Bloating and discomfort in the abdomen
- Unexplained weight loss
- Yellowing of the skin and whites of the eyes
- Light-colored stool, dark urine
- Itchy skin
- Fever, chills
- Worsening of the condition against the background of existing diabetes or diagnosis of diabetes
- Blood clots
- Fatigue
These symptoms should cause anxiety and become a reason to see a doctor.
Pain is the main and first sign of pancreatic cancer. It can be paroxysmal, strong or weak and occurs when the tumor has affected the nerves. Depending on the location of the malignant tumor of the pancreas, pain can be in the right hypochondrium if the head of the organ is affected, in the upper abdomen on the left if the tumor is in the body of the gland, or girdle pain if the entire pancreas is affected by cancer.
Pain in pancreatic cancer intensifies when the patient takes a horizontal position, as well as after eating, especially fatty and spicy food, after drinking alcohol. Often these symptoms are ignored or attributed to manifestations of other diseases, to the result of an improper diet, and medical help is not sought.
In some cases, pancreatic cancer can manifest itself as thrombosis of the veins of the legs, which causes pain, redness and swelling.
If a pancreatic tumor compresses the bile duct, it disrupts the outflow of bile and causes a complication - mechanical jaundice. In this case, the urine darkens and the stool becomes lighter, the skin, mucous membranes and sclera of the eyes acquire a yellowish tint, the liver and gallbladder increase in size, which causes the abdomen to increase in size, and itching of the skin appears. In advanced cases, jaundice can lead to liver or kidney failure, internal bleeding and even death.
If a malignant tumor disintegrates, substances from cancer cells enter the patient's blood, which lead to intoxication. This causes a decrease in appetite, sudden weight loss, weakness, lethargy, depression, apathy.
In some patients, a pancreatic tumor grows into the intestinal tissue. This leads to intestinal obstruction. If the splenic veins are compressed, this leads to an enlargement of the spleen. Damage to the endocrine functions of the pancreas can also lead to diabetes. And if the tumor grows into other organs, it can cause bleeding in them.
Our doctors

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services
Hormone therapy
Check-up
Immunotherapy Palliative care Orthopedic rehabilitation Cancer council Oncologist appointment Prevention of hair loss during chemotherapyRobotic surgery
Targeted therapy Genetic tests for cancer Biopsy under ultrasound guidance Second opinion in oncology Chemotherapy Endocrine therapy











































About the disease
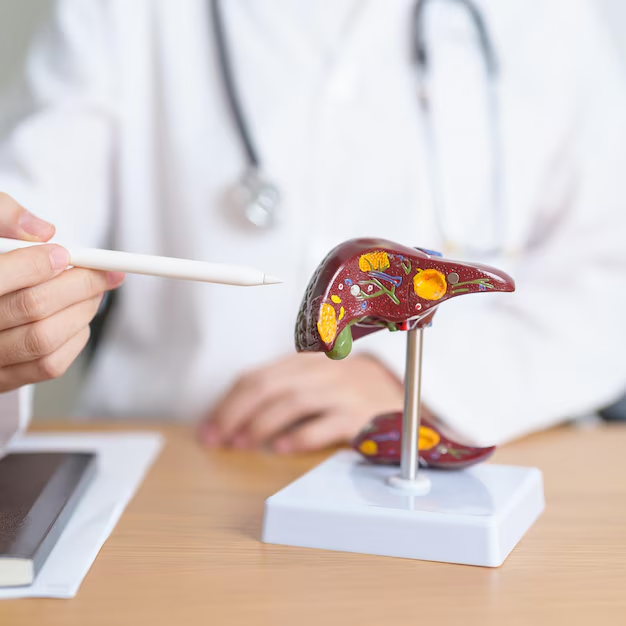
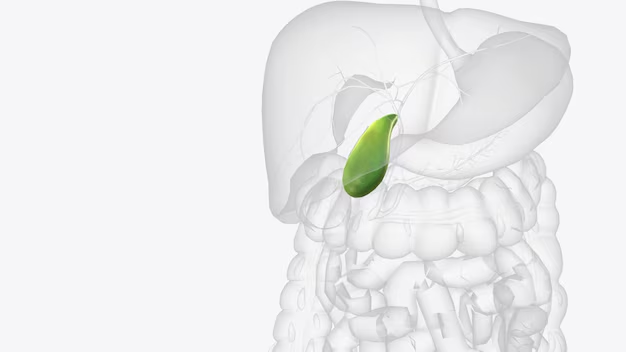
The pancreas is located in the left hypochondrium near the stomach and duodenum. It is penetrated by excretory ducts, vessels and nerves, covered with a connective tissue capsule and consists of three parts: the head, body and tail. The excretory duct connects with the bile duct in the head of the pancreas and opens into the duodenum.
When cells divide, mutations can appear in them, and some of these mutations can disrupt the functions of control over division. Then the cells begin to divide uncontrollably, and a tumor is formed.
Pancreatic cancer is one of the most aggressive types of cancer. It often proceeds asymptomatically until the late stages of the disease, when treatment becomes very difficult. With the bloodstream, cancer cells can spread throughout the body, forming distant secondary tumors (metastases).
The five-year survival rate (the percentage of patients who survive for five years after diagnosis) in the early stages of pancreatic cancer is up to 15%. This is because the organ is located in a place that is difficult to access for surgical operations and is tightly surrounded by other organs. The surgeon must have extensive experience in performing operations to remove a malignant tumor. And the risk of complications after surgery is very high.
Pancreatic cancer is the sixth most common cancer and is responsible for 7% of deaths from cancer of all types. It most often affects older people of both sexes. In more than half of the cases, the tumor develops in the head of the pancreas. And in almost a third of cases, the entire organ is affected.
Get examined at our clinic to identify diseases of the pancreas and other organs as quickly as possible.