Classification of myocardial infarction
- According to the anatomy of the lesion:
- transmural.
- intramural.
- subendocardial.
- subepicardial.
- By the extent of the lesion:
- large-focal (transmural), Q-infarction.
- Small-focal, non-Q heart attack.
- By localization:
- Myocardial infarction of the left ventricle (anterior, lateral, inferior, posterior).
- Isolated apical myocardial infarction.
- Myocardial infarction of the interventricular septum (septal).
- Myocardial infarction of the right ventricle.
- Combined localizations: postero-inferior, anterior-lateral, etc.
Clinical classification of myocardial infarction
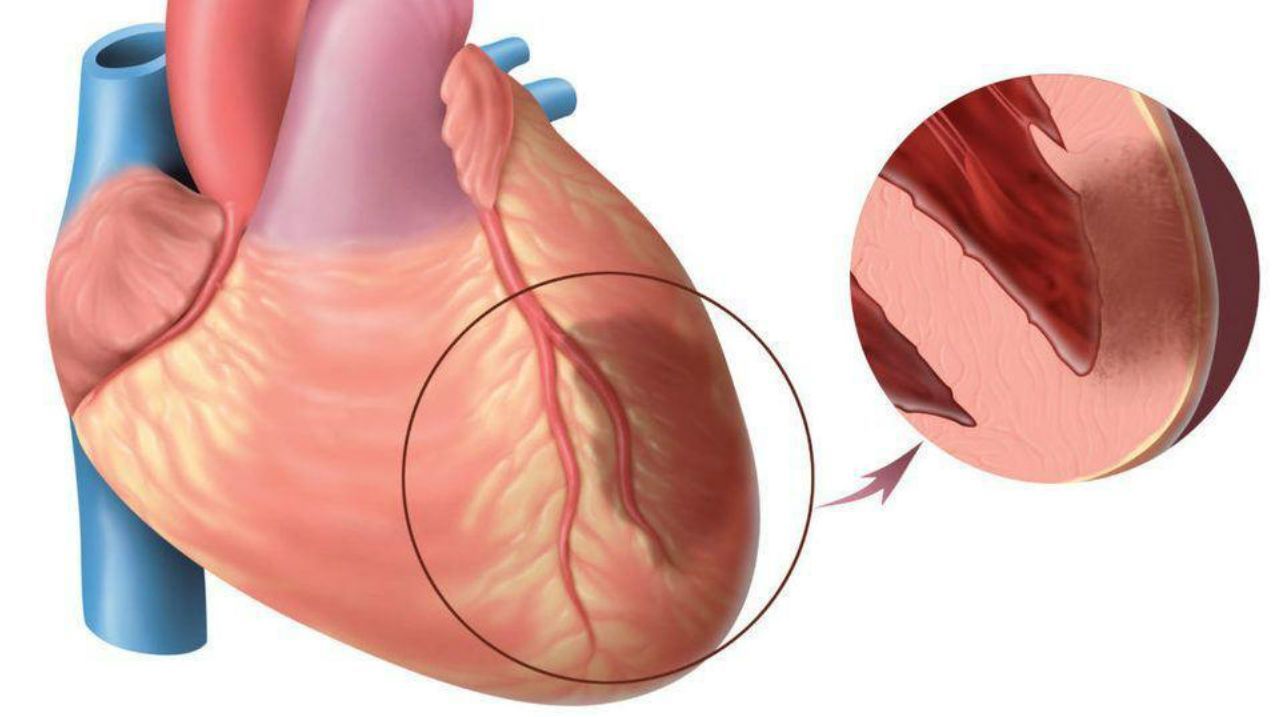
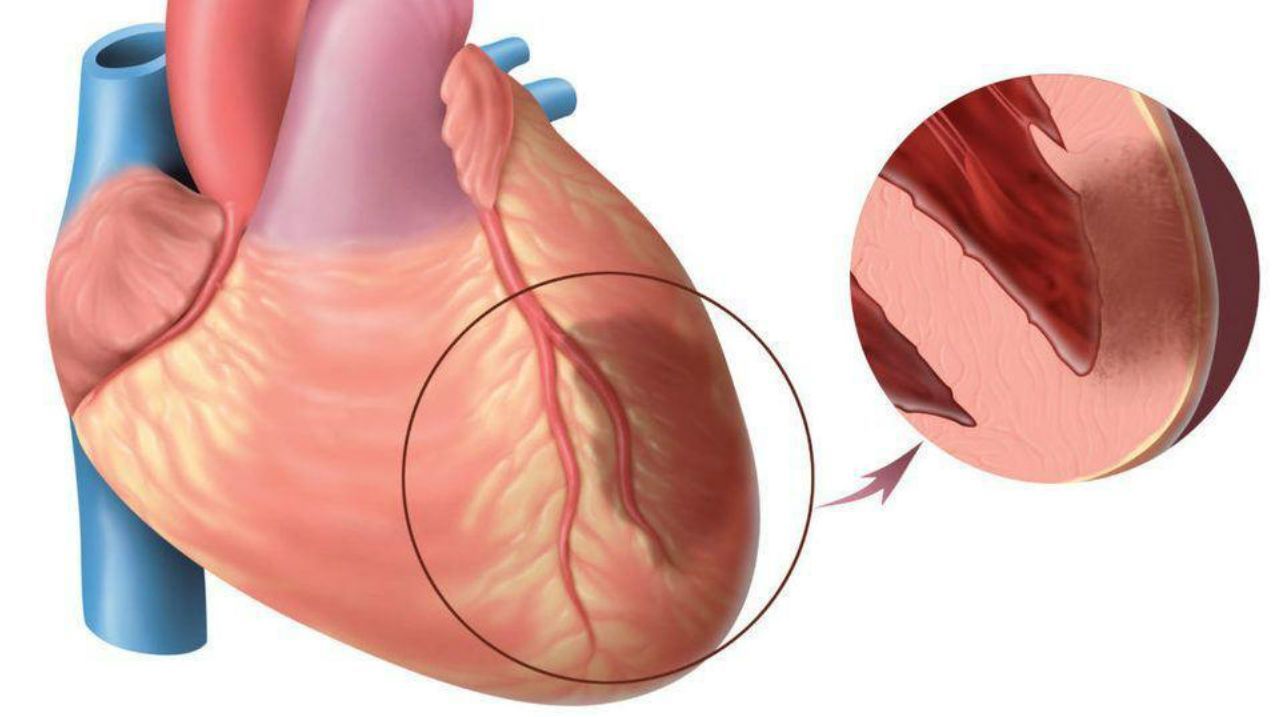
- Spontaneous MI (type 1) associated with ischemia due to a primary coronary event such as plaque erosion and/or rupture, fissure or dissection.
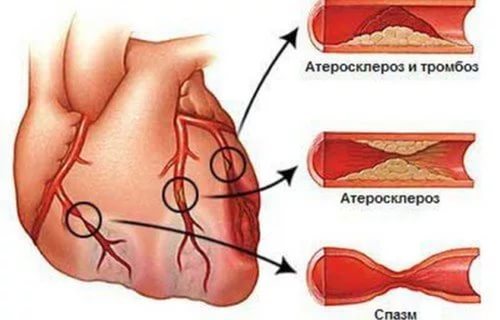
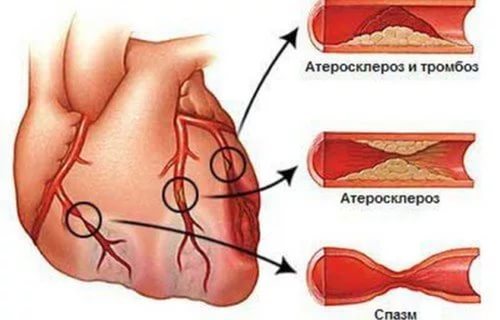
- Secondary MI (type 2) associated with ischemia caused by an increase in lack of oxygen or its supply, for example, in coronary spasm, coronary embolism, anemia, arrhythmia, hyper- or hypotension.
- Sudden coronary death (type 3), including cardiac arrest, often with symptoms of suspected myocardial ischemia with expected new ST elevation and new left bundle branch block, detection of a fresh coronary artery thrombus on angiography and/or autopsy, death occurring before receiving blood samples or before increasing the concentration of markers.
- PCI-associated MI (type 4a).
- MI associated with stent thrombosis (type 4b) confirmed by angiography or autopsy.
- CABG-associated MI (type 5).

Clinical picture of myocardial infarction
The most common and characteristic symptom of myocardial infarction is pain. In typical cases, the pain is diffuse in nature, localized in the left side of the chest, behind the sternum, can be given to the left arm, shoulder. Sometimes the pain is represented by a feeling of heaviness, burning, pressure. In rare cases, it is confused with pain in the stomach.
Most often, sensations last more than 30 minutes, are not stopped by taking nitroglycerin and painkillers, are accompanied by cold sweat, fear of death. Often the pains proceed in waves, for a long time, then weakening, then again intensifying. This pathology also has a number of atypical signs of a heart attack, which may indicate other problems. These include:
- Loss of consciousness.
- Irregular heart rhythm, including angina pectoris.
- Severe headache, dizziness that does not go away for several days.
- During an attack, nausea and fever are possible.
- Blue nasolabial triangle, etc.
Signs may be less or more pronounced, but the patient requires emergency ambulance and even being in intensive care. This is important to prevent deterioration, damage to other organs, such as the development of pulmonary edema, stroke as a result of insufficient oxygen supply to the brain, and other problems. The life of the patient depends on the correct and timely provision of qualified assistance. This is especially important during the first days. When the first signs appear, do not wait for them to last for a long time. MI is dangerous with a sharp deterioration and severe course with a high percentage of death. Therefore, you should seek medical help as soon as possible.
Atypical forms of myocardial infarction
In some cases, the symptoms of myocardial infarction may be atypical. There are the following forms of MI:
- Abdominal form - pain is localized in the upper abdomen, accompanied by bloating, nausea, vomiting.
- Asthmatic form - is represented by increasing shortness of breath, reminiscent of an attack of bronchial asthma.
- Atypical pain syndrome can be localized not in the chest, but in the right arm, shoulder, iliac fossa.
- Painless myocardial ischemia is rare, more often in patients with diabetes mellitus. In this case, sometimes hypotension, weakness, cyanosis of the lips can be noted in patients.
- The cerebral form is represented by dizziness, impaired consciousness, neurological symptoms.
- In some cases, in patients with osteochondrosis of the thoracic spine, the main pain syndrome in MI is accompanied by girdle pain in the chest, characteristic of intercostal neuralgia, which increases with a change in body position, palpation.
All complications of myocardial infarction are life-threatening:
- Cardiogenic shock.
- Heart break.
- Rhythm and conduction disorders (ventricular fibrillation).
- Acute heart failure.
- Left ventricular aneurysm development.
- Development of Dressler's syndrome.
- Development of chronic heart failure.
Myocardial infarction treatment
The only method of treating myocardial infarction, which in a significant part of cases completely prevents negative consequences and preserves the viability of the heart muscle, is the restoration of coronary blood flow in the first hours after the onset of the disease.
The patient needs urgent hospitalization in a hospital capable of immediate coronary angiography, balloon angioplasty and coronary artery stenting (surgical intervention). Restoration of blood flow in the coronary arteries is possible due to thrombolytic therapy (the first 6-12 hours of myocardial infarction), but this method is less effective and has its limitations.
Upon admission, an ECG (electrocardiography) is mandatory, in case of a mild condition, echocardiography, MRI, CT (computed tomography). Be sure to perform laboratory tests, including a biochemical blood test. A person's breathing is monitored (for the timely determination of a decrease or increase in frequency).
In the postinfarction period, the patient should also be under the supervision of the attending physician for several weeks or more (depending on the severity, lesion, concomitant diseases, etc.). Each stage of treatment is adjusted and, with the right approach, gives a high chance of a good recovery.
Myocardial infarction prevention
Under the prevention of acute myocardial infarction and other types, a system of measures is meant, the main focus of which is the prevention of atherosclerosis and the exclusion, if possible, of risk factors for myocardial infarction. The goal of prophylaxis after myocardial infarction is to prevent death, the development of recurrent myocardial infarction and chronic heart failure, and other possible complications.

Primary prevention of myocardial infarction is based on the observance of a "healthy lifestyle", following medical recommendations to prevent the development of coronary artery disease (maintaining normal levels of blood pressure, glucose, cholesterol). The patient must follow proper nutrition, regular physical activity and properly selected loads, give up bad habits.
Timely diagnosis of diseases that increase the risk of MI is also important. In the medical centers "K+31" you can undergo a complete examination to determine all health indicators and an accurate diagnosis. This helps to prevent the development of MI at any stage, including subacute, and also helps prevent other cardiac problems.
Secondary prevention after myocardial infarction is necessary to prevent death, the development of recurrent myocardial infarction and chronic heart failure. The long-term prognosis after MI is determined by the severity and prevalence of stenosing atherosclerosis of the coronary arteries; the degree of dysfunction of the left ventricle, the age of the patient, the presence of potentially dangerous arrhythmias.
After myocardial infarction, constant medical supervision is necessary to prevent the development of long-term complications of myocardial infarction (chronic heart failure, arrhythmias). These complications are in most cases successfully prevented with the appropriate regimen recommended by the doctor, nutrition and special drug treatment. It is recommended to regularly visit a cardiologist (at least once every 6 months) to monitor the general condition and assess the degree of effectiveness of the therapy.
It is important to remember that MI is a serious disease provoked by other diseases. Therefore, it is necessary to monitor the condition of all systems, including the endocrine system, regularly undergo a medical examination, and not ignore the medication prescribed by doctors. Sometimes simple pills can save a life, preventing the development of serious pathologies.